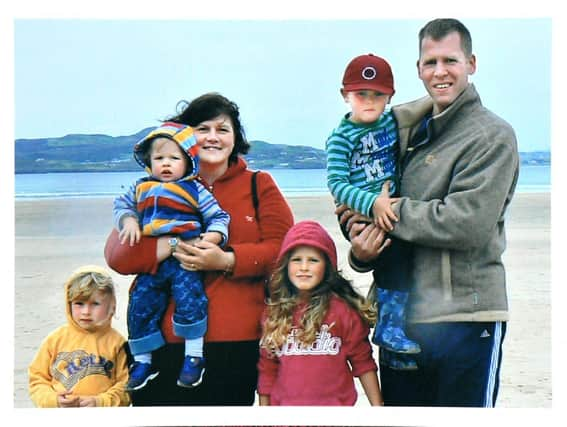
NI mum Joanne calls for dedicated Mother and Baby unit after postpartum psychosis ordeal

When Joanne’s son Joshua was 13 weeks old, she developed postpartum psychosis – a serious mental health condition following the birth of a baby, when the mother can experience hallucinations, delusions and mania and depression.
Unlike other regions of the UK, Northern Ireland does not have a dedicated mother and baby unit for mothers experiencing perinatal (during or after pregnancy) mental health issues, which means they are either admitted to a general acute psychiatric ward here for non-specialist treatment and separated from their babies (as Joanne was), or have to travel to another region of the UK.
Advertisement
Hide AdAdvertisement
Hide AdJoanne gave birth to Joshua, her fourth child, in 2008, and everything had been fine for the first few months after this birth.


She said: “Unfortunately the birthing experience in hospital with my third child had left me traumatised. I suffered horrendous neglect during labour and up until delivery I didn’t know if either of us would survive.
“In total contrast, and in a different hospital, Joshua’s birth could not have went better, which was such a relief for me. But at seven weeks old he was very ill and contracted bronchiolitis.
"He wasn’t breathing very well and needed urgent care so I had to take him to the hospital where I had been previously traumatised. He was admitted straight away and we were put into an insulation ward.
Advertisement
Hide AdAdvertisement
Hide Ad“I now know I was being triggered and started reliving my traumatic birth experience.
“I was petrified as I didn’t feel safe there - I didn’t sleep, I was worried sick about my baby and kept hyper vigilant to make sure Joshua was okay.
“Thankfully Joshua got better and we were discharged.”
It wasn’t until six weeks later during a visit to her parents for their wedding anniversary celebration that Joanne began to experience unusual symptoms.
“I started to feel really cold and suddenly my feet and legs went numb. I told my parents to call an ambulance. Soon I was completely paralysed and I was unable to speak.
Advertisement
Hide AdAdvertisement
Hide Ad“My mum thought I was having a stroke. I got blue-lighted to hospital - back to the one where I had been traumatised.
"My body went in and out of paralysis, I was hallucinating and my speech was incoherent. Something was badly wrong with my brain but the professionals had no idea what was going on.
"Soon I was displaying symptoms of mania and psychosis and had to be
sectioned and admitted to the local psychiatric ward.
“I clearly remember being surrounded by at least 12-15 members of staff, physically restrained, forcibly dragged and then thrown into a van that transported me to the locked ward.
Advertisement
Hide AdAdvertisement
Hide Ad"I must have been sedated as I woke up on the floor of the ward hanging onto the leg of a chair and the shoe laces of a male member of staff. I was a pathetic sight.
“I kept asking ‘where is my baby?’ but no one told me anything. I was terrified, helpless being separated from my family and now surrounded by all the other severely ill female patients.
"To say the experience was traumatic is an understatement, definitely not the proper place for an unwell mum to be who had recently given birth.
“General psychiatric facilities are totally inappropriate for women with postpartum psychosis as they require specialist diagnosis and treatment; plus their basic needs to be with, or even see, their babies are not provided for.
Advertisement
Hide AdAdvertisement
Hide Ad“I wasn’t given a diagnosis of postpartum psychosis back then only of manic depression (bipolar disorder), so more information would have been helpful for me to try and make sense of what had happened.
"It was during my recovery and finding Action on Postpartum Psychosis online that I first heard of postpartum psychosis and its connection to bipolar.”
Joanne is one of those calling for the establishment of a Mother and Baby psychiatric inpatient unit for Northern Ireland.
She said: “I firmly believe if I could have been treated in an MBU it would have been life-changing for me; speeding up my recovery as I could have been with my baby boy instead of constantly fretting for him.
Advertisement
Hide AdAdvertisement
Hide Ad"I was denied the opportunity to both care for my baby in those early weeks and have the chance to further develop the crucial mother and baby bond – something I still feel very guilty about 14 years on.”
Around 1,000 women each year in Northern Ireland will develop a severe postnatal illness. This can include postpartum psychosis, severe depression and anxiety, and obsessive compulsive disorder.
Between 84 and 122 will need admission to hospital.
Suicide is the leading cause of maternal death, but with the right care is almost always preventable.
Forty charities and organisations, including national and local organisations representing mothers, children and families, mental health charities and Royal Colleges have signed a letter to Health Minister Robin Swann, calling on the government to urgently prioritise an MBU.
Advertisement
Hide AdAdvertisement
Hide AdDr Jess Heron, chief executive of Action on Postpartum Psychosis said: ‘Members of our NI Peer Support group have talked about the distress of being separated from their babies, and how this has stayed with them, in some cases for many, many years.”